An Ukrinform reporter attended a unique heart surgery performed on a newborn just minutes after a cesarean section
The newborn’s heart is the size of a walnut. Born almost doomed, he was made fully healthy by the golden hands of Ukrainian surgeons.
When on the evening of November 18, Professor Ilya Yemets invited me to be present at a one-of-a-kind surgery the next morning, I stayed up all night from excitement. Of course, this was not because of air raid alerts. After all, tomorrow I will eyewitness something wholly incredible for any ordinary person to even imagine. Well, how is that?! The yet unborn child has a heart defect incompatible with life; nature has confused in places the aorta and the pulmonary artery — a congenital cardiac defect (deficiency in the septum between the aorta and the pulmonary artery) that effectively doomed the newborn to die within days after birth. … But that was not going to happen! Ukrainian cardiac surgeons will perform an extremely intricate surgery immediately after a cesarean section — for the first time globally! — to repair a cardiac deficiency with a jewelry-like precision, which will take just a few minutes for the tiny man to become healthy!

November 19. The thousandth day of the full-scale war. 8 am. Two large surgical teams. One is for obstetrics and gynecology, led by the director of the Kyiv Perinatal Center, Professor Dmytro Hovseyev, and the other for cardiac surgery, led by Professor Ilya Yemets, director of the Scientific and Practical Medical Center for Cardiology and Cardiac Surgery under the Ministry of Health.
The would-be mother holds her breath and concentrated, with excitement on her face. She is being prepared for surgery. The woman is on the verge of the miracle of giving birth to new life, but one can only assume what is happening in her soul. However, she completely trusts herself and her yet unborn baby under her heart to our doctors. The doctors are fully prepared and set for success.
… And, dare I say it, the thrill of a genuine symphony gets underway – a great beautiful creation, in this instance – an extremely complex surgical operation, performed by a well-played orchestra of doctors. In the operating room, everyone have their own role, everyone must play in tune, no one has the right to do wrong. Now they are all playing the same music, all working as a single organism.

Photo Director of the Kyiv Perinatal Center, Professor Dmytro Hovseev standing alongside Ilya Yemets, Director of the Scientific and Practical Medical Center for Cardiology and Cardiac Surgery under the Ministry of Health, Professor.
FOR THE FIRST TIME GLOBALLY, TEMPERATURE CONDITIONS IN CARIDAC OPERATING ROOM HAVE BEEN SET TO MIMIC THE TEMPERATURE OF WOMB
The history of cooperation between cardiac surgeon Yemets and obstetrician-gynecologist Hovseev in treating child patients with proven severe congenital cardiac defects began many years ago. In the perinatal center on Chornovola Street in Kyiv – in very close vicinity to the Cardiac Surgery Center – women in childbirth are operated on quickly, babies are delivered to a cardiac surgery unit as quickly as possible and a surgery is performed as soon as possible, which gives the child patient a chance to live. But before, it took hours, now it takes minutes. The distance between the two operating rooms is a few steps literally – in one the child is given birth, while in the other a life incompatible cardiac abnormality is immediately repaired. And this is what makes this surgery truly unique again – the creation of a “single medical space” integrating cardiac surgery and obstetrician-gynecology, this despite their different jurisdiction (the municipal perinatal center is administratively subordinated to Kyiv City’s municipal authorities, while Cardiac Surgery Center is under the authority of the Health Ministry.

For maximum comfort of the newborn, who feels warmth at 37-37.5 degrees Celsius while still in the womb, the “artificial womb” conditions were set up in the cardiac operating room in such a way that the baby feels like still in his mother’s womb. The little open bed, in which the child is immediately placed – is heated and maintains the set temperature, and the same temperature will be maintained in the operating room too. That is, temperature conditions in entire operating room will be set at the level to mimic the temperature conditions of the womb – and everyone engaged in the surgical process will work in it. Never before has this been done anywhere in the world, making it a truly historic event that will prevent many, very many risks.
When the obstetrician team finishes surgery on the mother, cardiac surgeons come into the process to do the main job – to perform cardiac surgery on the newborn.

THE BIRTH BABY IS BORN TO THE WORLD IN JUST TWO MINUTES AFTER CESAREAN CUT
The initial phase of this superb surgical work passes very quickly – as the saying goes, at the “allegro” pace. This is about a cesarean section. During 40 years of obstetric experience, Professor Hovseev has helped thousands of children to be born into this world. During his surgeries, some 5-7 minutes usually pass between the moments the cesarean cut is made and the baby comes into this world. Now this time has been reduced to just two minutes! The little head appears. It’s a boy weighing 3,300. The first cry of a new life born into the world. He is here, here with us and in safe hands.
Being an ordinary person, I took these first sounds from a newborn as a good sign – he is strong, he will be able to overcome all the odds. But doctors explained that, in fact, such a loud “declaration” about his own birth was made possible solely thanks to the remnants of the oxygen the baby received from his mother while still unborn. After one minute, the baby’s oxygen supply rans out, signs of decompensation began to appear, the saturation becomes critically low – the baby patient stops breathing on his own and crying…

THE PATIENT HAS TWO CIRCLES OF BLOOD CIRCULATION WHICH ARE RUNNING IN PARALLEL SEPARATED FROM EACH OTHER
While you, the readers, are holding your breath and the surgeons are confidently approaching the next, second part of their life symphony, I will tell you about the cardiaс deficiency the child was born with. It is called “transposition of the great vessels associated with an obscured ventricular septal defect due to an abnormal systemic atrioventricular valve”. The pregnant woman has foreign citizenship, the cardiac defect was diagnosed on an ultrasound scan in Moldova, and, when 37 weeks pregnant, she first visited Ukraine, where the defect was confirmed and a serious side defect was found – fetal restriction of foramen ovale — a serious disorder of the fetus that can be associated with fetal hydrops, arrhythmias, and other signs of major fetal compromise. So an urgent surgical intervention was required. Ukrainian doctors developed a customized treatment plan and scheduled a surgery.

Photo Oleksandr Teterin, chief of perinatal diagnostics unit, is weighing the newborn
Head of the Perinatal Diagnostics Unit, Oleksandr Teterin, who accompanied the newborn during the surgery, explained what transposition of the great arteries is. It is a reversal of the aorta and pulmonary artery, the two major blood vessels leaving from the heart. In D-type transposition of the great arteries (D-TGA), the two main arteries (aorta and pulmonary artery) are connected to the wrong chambers of the heart. When the vessels are switched, the aorta is on the wrong side of the heart and gets oxygen-poor blood from the body instead of oxygen-rich blood fresh from the lungs. The oxygen-poor blood continues to recirculate to the body. At the same time, the pulmonary artery keeps recirculating oxygen-rich blood to the lungs instead of sending it out to the body. This heart defect will require surgery.
Patent foramen ovale (PFO) is a hole between the left and right atria (upper chambers) of the heart. This hole exists in everyone before birth, but most often closes shortly after being born. PFO is what the hole is called when it fails to close naturally after a baby is born.This works as a valve that directs blood from the lower half of the fetus’s body to the upper chambers, bypassing the non-functioning lungs. After birth, the lungs begin to breathe – the pressure between the atria changes and the oval window closes. Infants with D-TGA and no other heart defects do not have symptoms. It’s OK unless not found along other heart abnormalities. When associated with an obscured ventricular septal defect, it can be life threatening, because the patient has two circles of blood circulation which are running independently of each other in parallel, but not in sequence. That is, oxygen-rich blood does not recirculate to the body, and the blood already circulating does not give off carbon dioxide through the lungs as it should, because it does not travel there. As long as the foramen ovale remains unclosed, mixing occurs, where oxygenated blood gets into unsaturated blood. Overall, blood flow is normal and the condition does not require an operation. But when the “window” closes (which happens much earlier to children patients with this abnormality), mixing no longer occurs and the patient dies. But thanks to this surgery, this will not be the case.

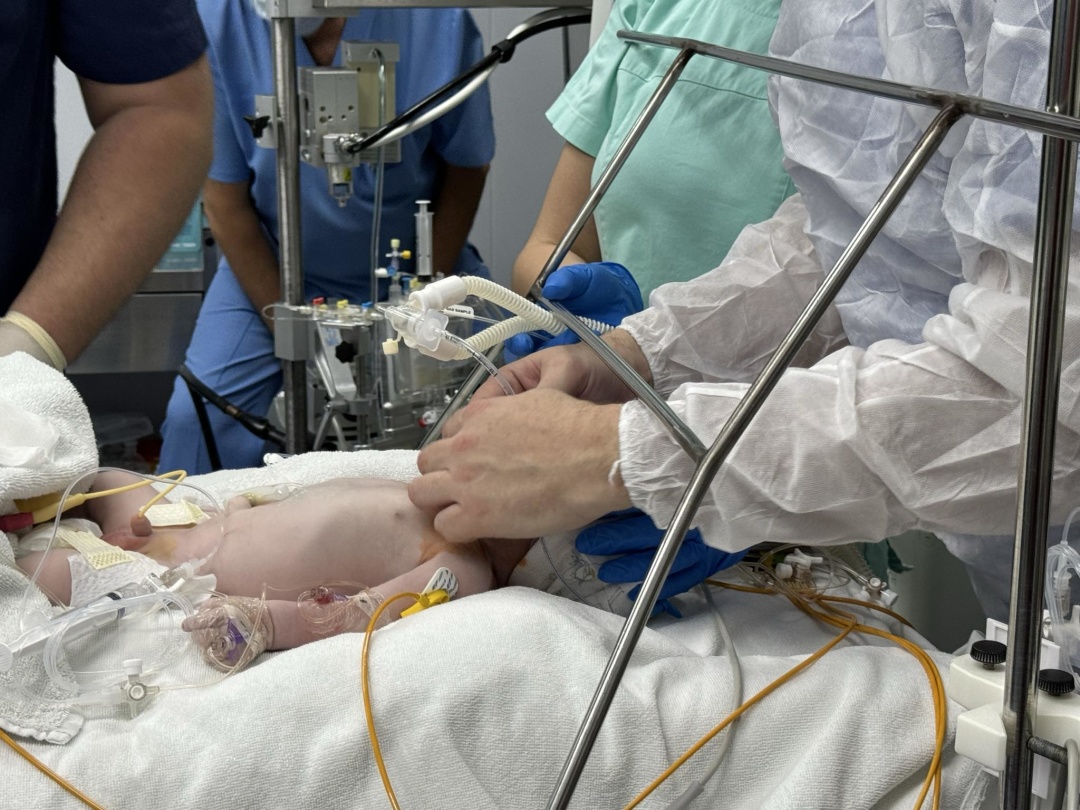
THE BABY WAS PUT ON ARTIFICIAL PULMONARY VENTILATION, STABILIZED, WARMED AND CONNECTED TO ARTIFICIAL BLOOD CIRCULATION
The surgeons commence the second part of the life symphony – the “rondo”.
This is the initial stabilization of the newborn in the operating room. The patient is in severe condition that requires resuscitation. Ivan Anikin, the head of the anesthesiology and neonatal intensive care unit at the Kyiv City Municipal Children’s Hospital No. 2, assisted by the obstetric team, puts the newborn patient on artificial pulmonary ventilation, stabilizes the heart disorders, warms him up and transfers to the operating room for artificial blood circulation.
The doctor says that if this newborn baby had been born in a maternity hospital far away from a cardiology clinic, then most likely, even after Rashkind balloon atrial septostomy procedure, such a young patient would be far more difficult and risky to get stabilized for transportation. This would have required additional preventive stabilization surgery before performing the main cardiac surgery to correct the defect. If the time of transportation is too long, the probability is high that the patient will not survive it… And we managed to avoid additional preventive surgery and procedures, and immediately proceeded to the main surgery.
THE PATIENT’S AGE – FROM UMBILICAL CORD CUTTING TO CONNECTION TO HEART-LUNG MACHINE – IS NUMBERED IN MINUTES
Part 3 – Minuet.
This part of the surgery is performed in the cardiac operating room. Emergency therapy for an infant patient with transposition of the great vessels consists of setting up a sufficient oxygen level and ensuring sustainable hemodynamics of cardiac and pulmonary activity. The patients age – from the moment the umbilical cord is cut to the moment the patient is connected to an artificial heart-lung machine – is numbered in minutes.
It is crucial that the artificial blood circulation machine uses the patient’s own umbilical cord blood rather than donor blood, a method first introduced globally by Ilya Yemets in 2009. That is, the newborn receives own blood, which contains vital biologically active substances, including growth hormones and placental proteins, including regenerative and immunomodulatory proteins.

Working at the operating table is the prominent cardiac surgeon Ilya Yemets, assisted by his surgery team. I am present in the same room, and on the monitor in the operating room I can see with my own eyes all the most delicate manipulations that they perform. An open tiny heart under the virtuoso hands of great people! At the beginning, the color of the child’s heart, which is the size of a small walnut, is dark lilac, close to blue with a reddish tint, after being enriched with oxygen-rich blood, it brightens before your eyes and changes color to a delicate pink! An unforgettable impression of the appearance of this barely smoldering pulse of life, a tiny heart that will very soon beat at full strength.

IN SUCH A SURGERY, THE PATIENT’S HEART CAN BE STOPPED FOR UP TO AN HOUR. AFTER THE SURGERY, THE NEWBORN BABY WILL BE FULLY HEALTHY
Part 4 – Rondo.
This is the Climax. The most technically sophisticated part of the surgery, which takes several hours to complete.
Professor Yemets performs an arterial switch procedure to repair d-transposition of the great arteries; the aorta and pulmonary artery are cut in half, the surgeon puts the baby’s aorta and pulmonary artery in the correct places. Without involving the heart valves, the surgeon disconnects these major blood vessels and attaches them to the correct heart chambers. The cut off section of the aorta is sewn to this area, and then a tube is made from a piece of the patient’s own pericardium, which is then sewn into the new pulmonary artery, restoring it as well. Now everything is normal: the main vessels are leaving from the ventricles from which they are intended to leave. During this part of the surgery, the child’s heart is stopped. Even as I write these lines, I cannot believe the reality of what I have seen! The shorter the time the heart is without blood flow, the better the chance of recovery, but during this sort of surgery, it can be deprived of oxygen for up to an hour (!), because this is an extremely sophisticated cardiac surgery that requires the application of lots of stitches with jewelry-like precision.

Photo Cardiac surgeon Ilya Yemets at work
Transposition of the great vessels associated with an obscured ventricular septal defect is an abnormality that carries a fairly low risk of any other abnormalities, including genetically induced ones. The arterial switch surgery reconstructs the heart to work the way it should, both anatomically and functionally. Long-term cardiac function should be excellent, the child will have normal ventricular function and will not have heart rhythm disorders. That is, he will be fully healthy and will be able to play sports.
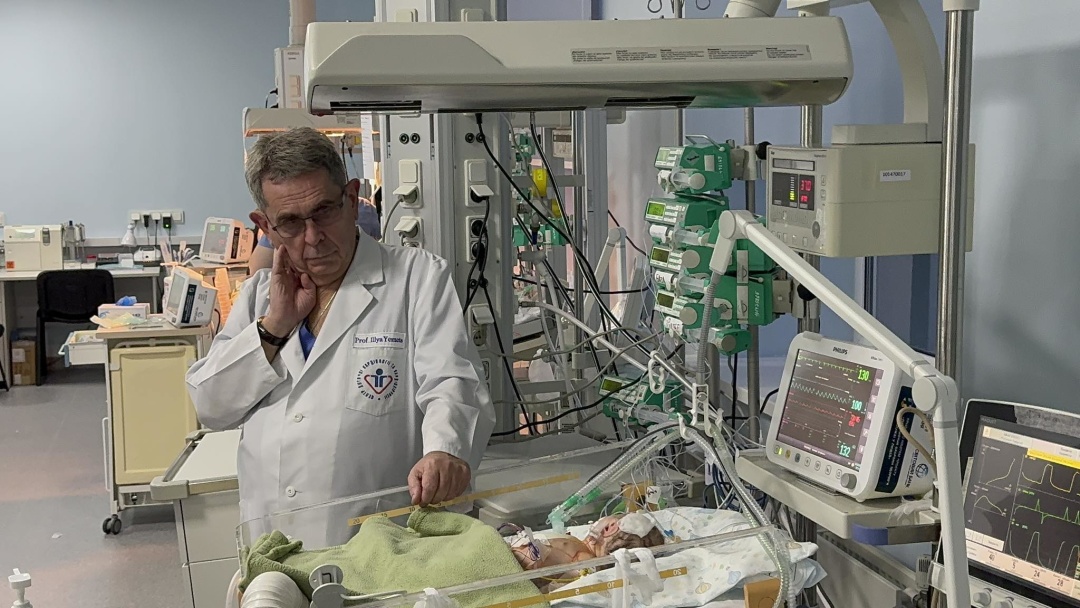
Photo Ilya Yemets in intensive care ward
Final. The surgical team have performed brilliantly
The little patient was transferred to intensive care, where he will spend 5-7 days before being placed under observation at the Center’ unit for a few more days. Afterwards the patient will be let go home in Moldova, accompanied by his mother and father, and will differ in no way from other healthy peers. Except that a small scar will remain on his chest, a reminder of the incredible miracle performed by Ukrainian cardiac surgeons, who even now, during the terrible war where Russia is seeking to get us erased from the face of the earth, are performing miracles like that.

Photo Little Luka with his parents
When I was finishing this article, I was made known that the boy was named Luka, and he is already being prepared for discharge. Be happy, little one! And may the war and those who unleashed it be cursed.
Lyubov Baziv. Kyiv
Photo via Author and Oles Yanchuk
P.S.
Overnight on November 19, Russian military fired a wave of 87 Shahed one-way attack drones at Ukraine, along with unmanned aerial vehicles of an unknown class.
November 19: 12 civilians sustained injuries in the aftermath of a drone strike on Kharkiv city; a day of mourning was declared in Odesa and the region for the 10 people killed in a Russian attack involving a duo of Iskander-M ballistic missiles.
Source: A Life Symphony Performed by Ukrainian Surgeons on The 1,000th Day of the War




